Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Types of Blisters on the Feet

Blisters are fluid-filled sacs that form on the skin due to friction, heat, or cold. They commonly develop on the feet as the result of running, wearing ill-fitting shoes, or exposure to extreme temperatures. Blisters caused by friction typically appear as raised, clear bubbles of fluid on the skin, while those caused by heat or cold may be accompanied by redness, swelling, or pain. Symptoms include a painful, tender area where the skin has been damaged. Blisters from heat can occur from burns, while cold blisters may form due to frostbite or prolonged exposure to cold surfaces. The pain can range from mild to intense, especially when pressure is applied. A podiatrist can help by providing proper treatment, such as draining the blister, if necessary, dressing it to prevent infection, and advising on how to avoid future blisters. They can also offer guidance on selecting the right footwear. If you have painful blisters on the feet, it is suggested that you schedule an appointment with a podiatrist.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact one of our podiatrists of Dr. Jeffrey J. Betman & Associates . Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our offices located in Northwest Chicago, Southwest Chicago, and Wicker Park, Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters on the Feet
Blisters are a common ailment of people who wear shoes that are either too tight or rub against the feet in an uncomfortable way. Knowing the basics of blisters is important for understanding how they are formed and what treatments should be used for them.
A blister on the foot, or any other part of the body, is a small pocket that is filled with fluid. It usually forms on the upper layer of the skin because these layers are loose enough to allow a blister to form. The most common fluid in a blister is just a clear, watery-like fluid that usually isn’t cause for concern. However, blisters can fill up with blood if they are deep enough and pus if they have become infected with bacteria.
Blisters almost always form on the feet due to shoes rubbing up against the foot, where the friction causes blisters. These can occur after you have walked for a long period of time or when your shoes do not fit you properly. Your feet are also more prone to blisters if they are moist, so keeping them dry and clean is one preventative step you can take.
Preventing infection should be the number one concern when treating blisters, as well as relieving the pain they can cause. Using a bandage to cover up the blister will help it heal and prevent bacteria from entering it. New skin will form under the blister and eventually cause it to pop. You can also take a sterilized pin and try to pop it yourself.
If the blister is filled with pus or blood, seeking treatment from a doctor is ideal. Antibiotics may need to be taken in order to completely eliminate the bacteria inside the blister. See a doctor to have an antibiotic prescribed.
The best way to treat blisters is to prevent them all together. Keeping your feet dry and making sure that your shoes fit properly are just two of the steps you can take to prevent blisters. Shoes that are too tight or shoes that are too loose and allow your feet to slide in them will cause blisters. Applying a bandage to an area where you think a blister is about to form is another way you can prevent them.
How to Manage a Broken Foot

A broken foot can result from direct impact, falls, crush injuries, or repetitive stress. Symptoms include pain, swelling, bruising, limping, and difficulty bearing weight. The severity of a foot fracture depends on which of the 26 bones in the foot is affected. A podiatrist can diagnose your injury using X-rays or advanced imaging such as a CT scan. Treatment may involve immobilization with a stiff-soled shoe, boot, or brace to support healing. Some fractures, particularly those that involve joint surfaces or cause displacement, may require surgery to restore alignment. One possible complication of a foot fracture is non-union, which occurs when a broken bone fails to heal properly due to poor blood supply, continued movement at the fracture site, or other factors. This can lead to chronic pain and instability in the foot. Other complications include arthritis, if a joint is involved, and infection if the skin is broken. Recovery time depends on the type and location of the fracture. If you have a broken foot bone, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options, which may include surgery.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Dr. Jeffrey J. Betman & Associates . Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Northwest Chicago, Southwest Chicago, and Wicker Park, Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Causes and Risk Factors for PAD
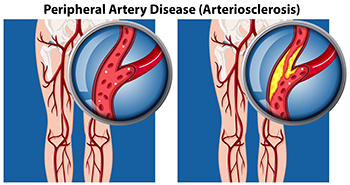
Peripheral artery disease, or PAD, occurs when plaque builds up in the arteries, causing reduced blood flow to the lower limbs. This leads to such symptoms as pain, cramping, or numbness in the feet, toes, or ankles. Smoking, diabetes, high blood pressure, and high cholesterol are major risk factors, while aging and a family history of vascular disease can also contribute to its development. Poor circulation from PAD may cause slow-healing wounds, skin discoloration, and, in severe cases, ulcers that increase the risk of infection or limb loss. A podiatrist can evaluate the blood flow to the feet and ankles, identify complications, and recommend appropriate treatment to help prevent more serious outcomes. Depending on the severity of the peripheral artery disease, treatment may include medical management or procedures like angioplasty or bypass surgery. If you are experiencing foot problems related to peripheral artery disease, it is suggested that you visit a podiatrist for guidance and treatment options.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Dr. Jeffrey J. Betman & Associates . Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Northwest Chicago, Southwest Chicago, and Wicker Park, Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Keep Your Feet Healthy So You Can Stay Active
Ingrown Toenails

Ingrown toenails occur when the edges or corners of a toenail grow into the surrounding skin, causing pain, swelling, and sometimes infection. This condition commonly affects the big toe and can result from improper nail trimming, tight shoes, or injury. Symptoms of ingrown toenails include redness, tenderness, swelling, and sometimes a discharge of pus if an infection develops. The pain can range from mild to severe, making it difficult to wear shoes or walk comfortably. A podiatrist can help treat ingrown toenails by removing the affected portion of the nail or, in more severe cases, performing a minor surgical procedure to prevent it from recurring. They can also provide advice on proper nail care and footwear to prevent future issues. If you are dealing with ingrown toenails, it is suggested that you make an appointment with a podiatrist.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact one of our podiatrists of Dr. Jeffrey J. Betman & Associates . Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our offices located in Northwest Chicago, Southwest Chicago, and Wicker Park, Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.